nonpeptide organic molecules that have antibiotic activity.
Among these agents are enzymes that digest microbial cell
walls, peptides and a protein that damages microbial mem-
branes, and the small organic molecules phytoalexins. The
importance of the phytoalexins is shown by the fact that mu-
tations that alter their biosynthetic pathways result in loss of
resistance to many plant pathogens. In some cases, the re-
sponse of plants to pathogens goes beyond this chemical as-
sault to include an architectural response, in which the plant
isolates cells in the infected area by strengthening the walls of
surrounding cells. Table 1-4 compares the capabilities of im-
mune systems in a wide range of multicellular organisms,
both animals and plants.
Immune Dysfunction and
Its Consequences
The above overview of innate and adaptive immunity depicts
a multicomponent interactive system that protects the host
from infectious diseases and from cancer. This overview
would not be complete without mentioning that the immune
system can function improperly. Sometimes the immune sys-
tem fails to protect the host adequately or misdirects its ac-
tivities to cause discomfort, debilitating disease, or even
death. There are several common manifestations of immune
dysfunction:
■
Allergy and asthma
■
Graft rejection and graft-versus-host disease
■
Autoimmune disease
■
Immunodeficiency
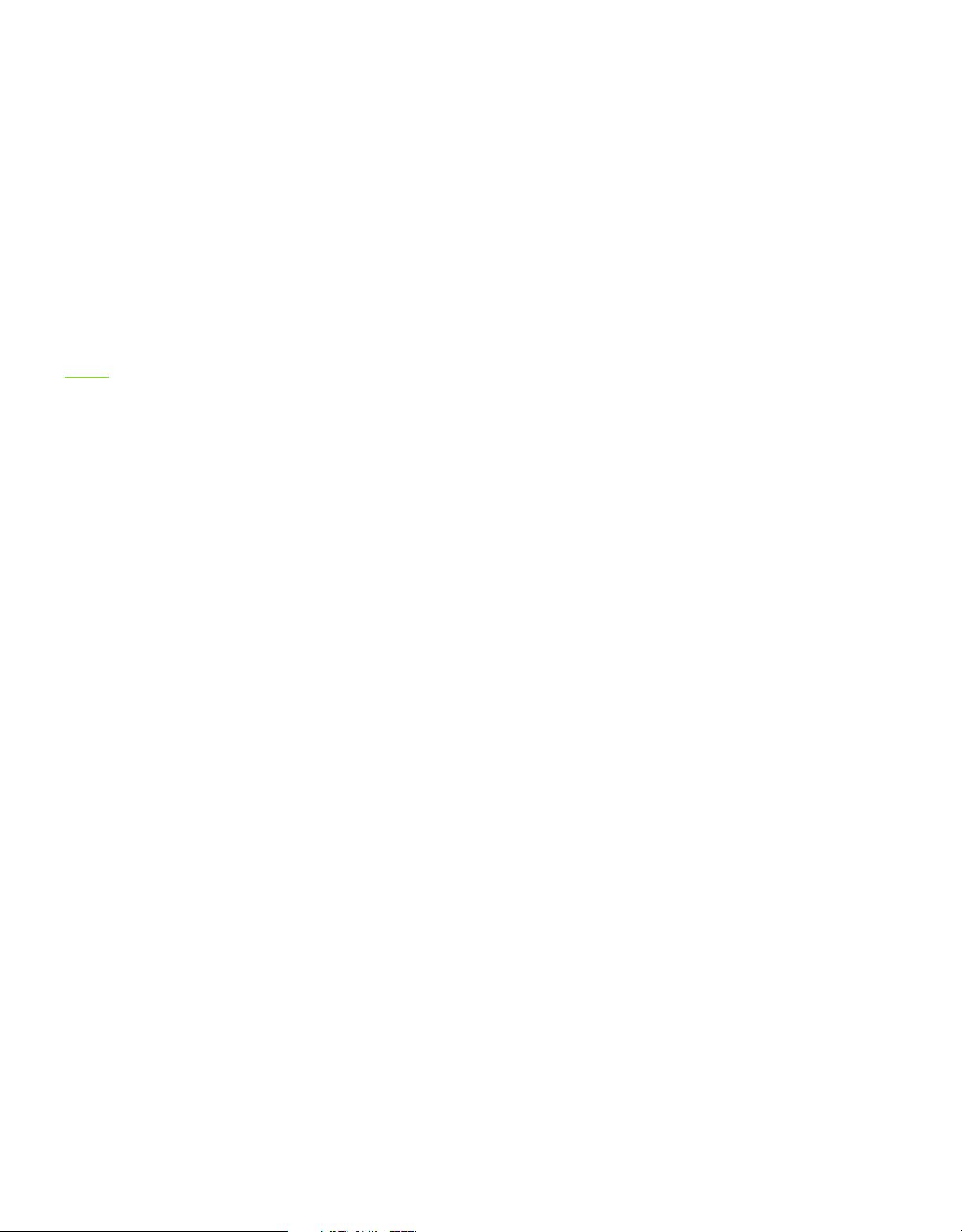
Allergy and asthma are results of inappropriate immune re-
sponses, often to common antigens such as plant pollen,
food, or animal dander. The possibility that certain sub-
stances increased sensitivity rather than protection was rec-
ognized in about 1902 by Charles Richet, who attempted to
immunize dogs against the toxins of a type of jellyfish,
Physalia. He and his colleague Paul Portier observed that
dogs exposed to sublethal doses of the toxin reacted almost
instantly, and fatally, to subsequent challenge with minute
amounts of the toxin. Richet concluded that a successful im-
munization or vaccination results in phylaxis, or protection,
and that an opposite result may occur—anaphylaxis—in
which exposure to antigen can result in a potentially lethal
sensitivity to the antigen if the exposure is repeated. Richet
received the Nobel Prize in 1913 for his discovery of the ana-
phylactic response.
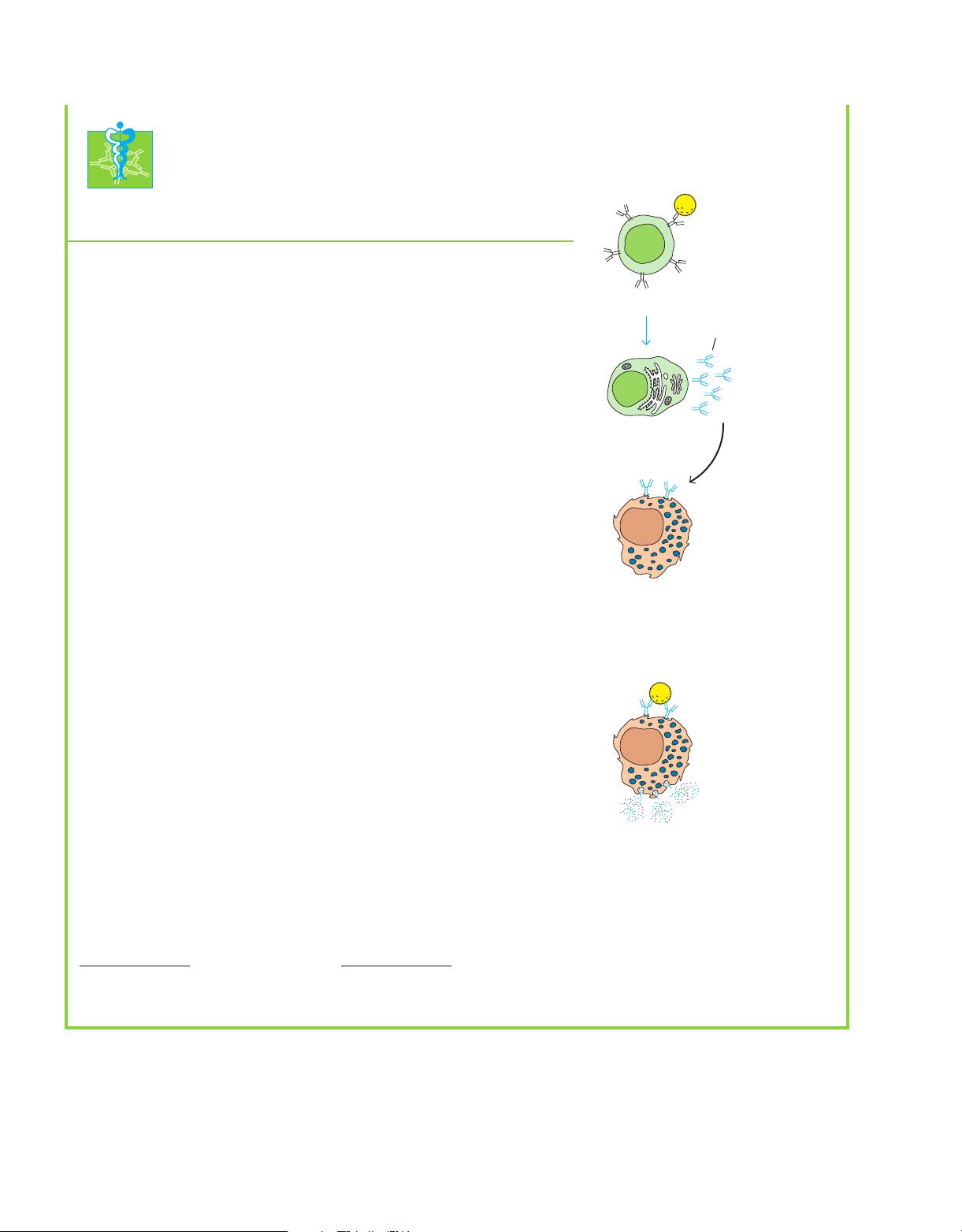
Fortunately, most allergic reactions in humans are not
rapidly fatal. A specific allergic or anaphylactic response usu-
ally involves one antibody type, called IgE. Binding of IgE to
its specific antigen (allergen) releases substances that cause
irritation and inflammation. When an allergic individual is
exposed to an allergen, symptoms may include sneezing,
wheezing, and difficulty in breathing (asthma); dermatitis or
skin eruptions (hives); and, in more extreme cases, strangu-
lation due to blockage of airways by inflammation. A signifi-
cant fraction of our health resources is expended to care for
those suffering from allergy and asthma. The frequency of
allergy and asthma in the United States place these com-
plaints among the most common reasons for a visit to the
doctor’s office or to the hospital emergency room (see Clini-
cal Focus).
When the immune system encounters foreign cells or tis-
sue, it responds strongly to rid the host of the invaders. How-
ever, in some cases, the transplantation of cells or an organ
from another individual, although viewed by the immune
system as a foreign invasion, may be the only possible treat-
ment for disease. For example, it is estimated that more than
60,000 persons in the United States alone could benefit from
a kidney transplant. Because the immune system will attack
and reject any transplanted organ that it does not recognize
as self, it is a serious barrier to this potentially life-saving
treatment. An additional danger in transplantation is that
any transplanted cells with immune function may view the
new host as nonself and react against it. This reaction, which
is termed graft-versus-host disease, can be fatal. The rejec-
tion reaction and graft-versus-host disease can be suppressed
by drugs, but this type of treatment suppresses all immune
function, so that the host is no longer protected by its im-
mune system and becomes susceptible to infectious diseases.
Transplantation studies have played a major role in the de-
velopment of immunology. A Nobel prize was awarded to
Karl Landsteiner, in 1930, for the discovery of human blood
groups, a finding that allowed blood transfusions to be car-
ried out safely. In 1980, G. Snell, J. Dausset, and B. Benacerraf
were recognized for discovery of the major histocompatibil-
ity complex, and, in 1991, E. D. Thomas and J. Murray were
awarded Nobel Prizes for advances in transplantation immu-
nity. To enable a foreign organ to be accepted without sup-
pressing immunity to all antigens remains a challenge for
immunologists today.
In certain individuals, the immune system malfunctions
by losing its sense of self and nonself, which permits an im-
mune attack upon the host. This condition, autoimmunity,
can cause a number of chronic debilitating diseases. The
symptoms of autoimmunity differ depending on which
tissues and organs are under attack. For example, multiple
sclerosis is due to an autoimmune attack on the brain and
central nervous system, Crohn’s disease is an attack on the
tissues in the gut, and rheumatoid arthritis is an attack on
joints of the arms and legs. The genetic and environmental
factors that trigger and sustain autoimmune disease are very
active areas of immunologic research, as is the search for im-
proved treatments.
If any of the many components of innate or specific im-
munity is defective because of genetic abnormality, or if any
immune function is lost because of damage by chemical,
physical, or biological agents, the host suffers from immu-
nodeficiency. The severity of the immunodeficiency disease
18
PART I
Introduction
8536d_ch01_001-023 8/1/02 4:26 PM Page 18 mac79 Mac 79:45_BW:Goldsby et al. / Immunology 5e: