2.1. Heart beat period and QRS detection 10
rhythms are characteristic for HRV signals and have been related to, e.g., humoral factors such as the
thermoregulatory processes and renin-angiotensin system [5].
Heart rate variability (HRV) is a commonly used tool when trying to assess the functioning of cardiac
autonomic regulation. It has been used in multitude of studies, related to cardiovascular research and
different human wellbeing applications, as an indirect tool to evaluate the functioning and balance of the
autonomic nervous system (ANS) [51].
One of the main clinical scenarios where HRV has been found valuable include the risk stratification
of sudden cardiac death after acute myocardial infarction [51, 1, 22, 42]. In addition, decreased HRV
is generally accepted to provide an early warning sign of diabetic cardiovascular autonomic neuropathy
[51, 1], the most significant decrease in HRV being found within the first 5-10 years of diabetes [55, 48].
Besides these two main clinical scenarios, HRV has been studied with relation to several cardiovascular
diseases, renal failure, physical exercise, occupational and psychosocial stress, gender, age, drugs,
alcohol, smoking and sleep [54, 27, 51, 43, 2, 1].
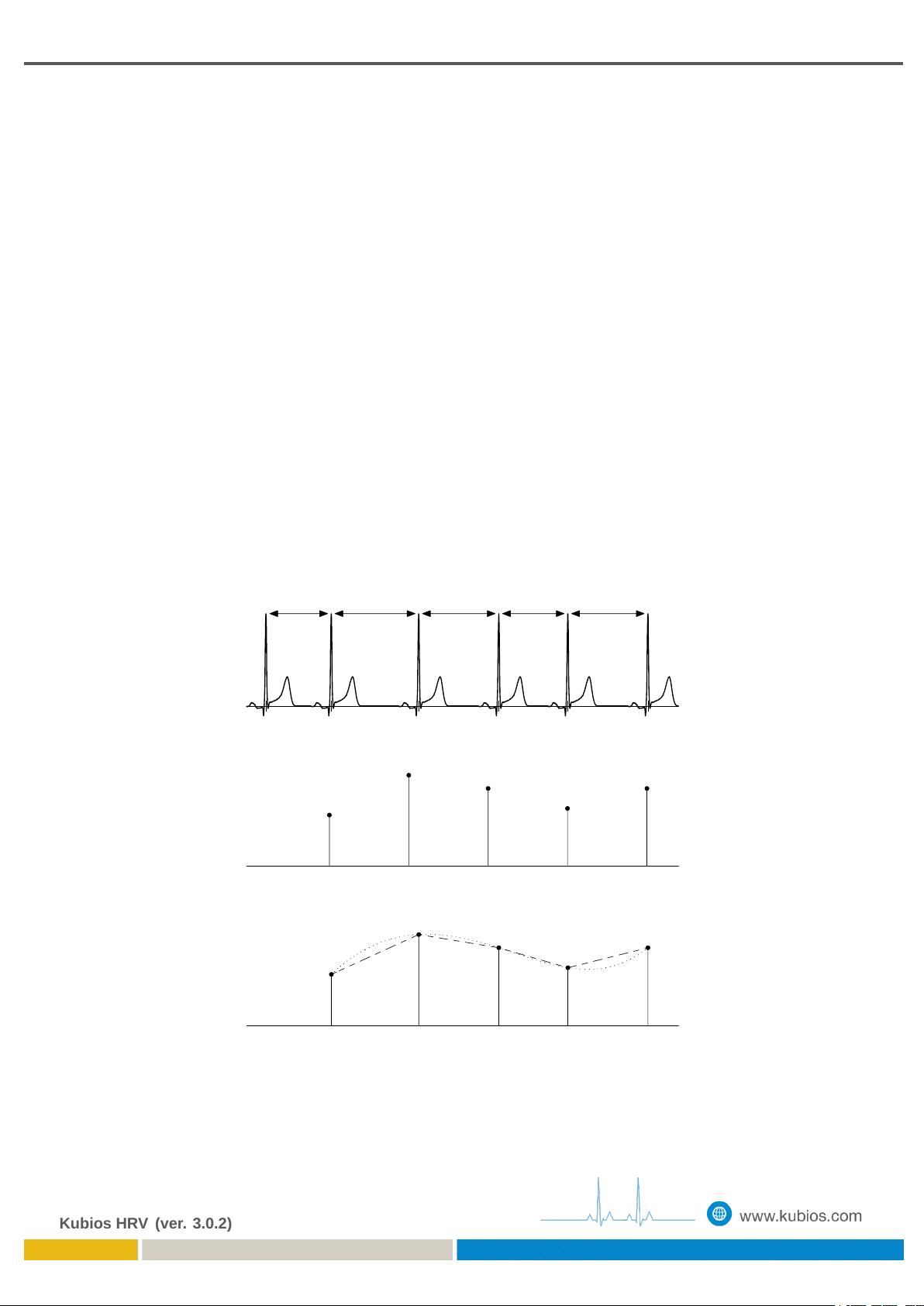
The term HRV refers, in general, to changes in heart beat interval which is a reciprocal of the heart
rate. This is also the case here. The starting point for HRV analysis is the ECG recording from which
the HRV time series can be extracted. In the formulation of the HRV time series, a fundamental issue is
the determination of heart beat period.
2.1 Heart beat period and QRS detection
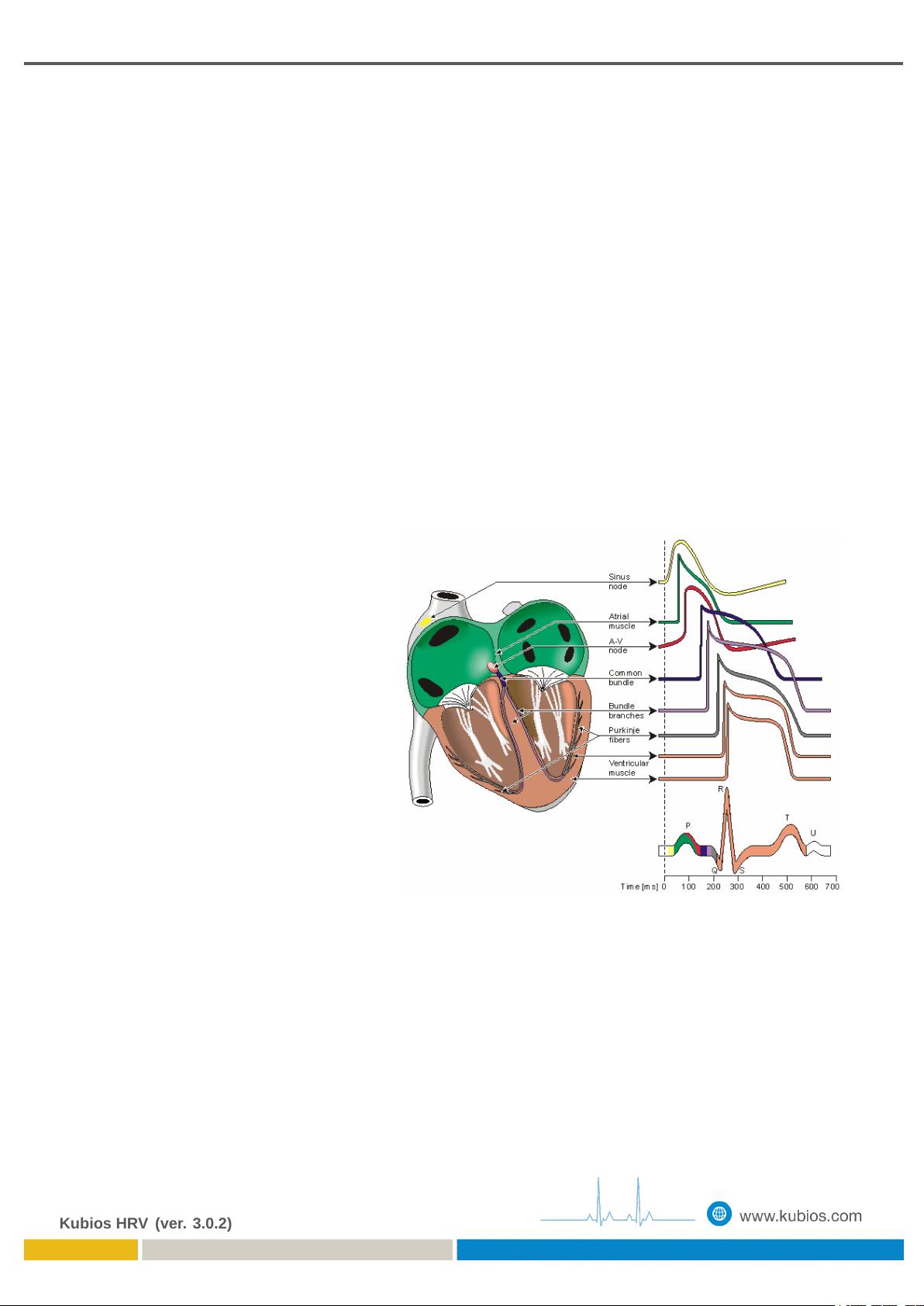
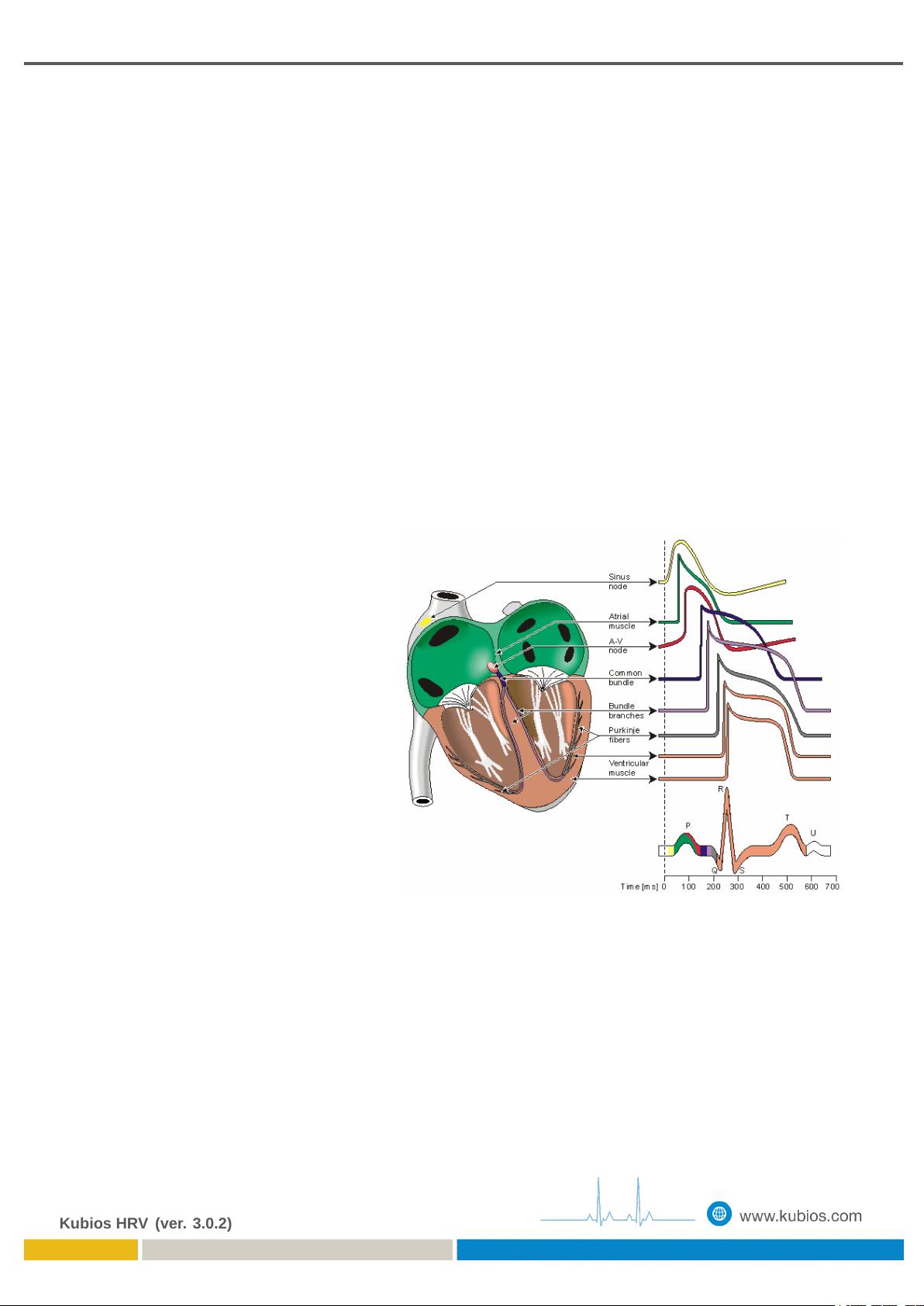
The aim in HRV analysis is to exam-
ine the sinus rhythm modulated by the
autonomic nervous system. Therefore,
one should technically detect the occur-
rence times of the SA-node action po-
tentials. This is, however, practically
impossible and, thus, the fiducial points
for the heart beat is usually determined
from the ECG recording. The near-
est observable activity in the ECG com-
pared to SA-node firing is the P-wave
resulting from atrial depolarization (see
Fig. 2.2) and, thus, the heart beat pe-
riod is generally defined as the time
difference between two successive P-
waves. The signal-to-noise ratio of the
P-wave is, however, clearly lower than
that of the strong QRS complex which
results primarily from ventricular depo-
larization. Therefore, the heart beat
period is commonly evaluated as the
time difference between the easily de-
tectable QRS complexes.
A typical QRS detector consists of a
preprocessing part followed by a deci-
sion rule. Several different QRS de-
tectors have been proposed within last
decades [52, 36, 37, 20, 14].
Figure 2.2: Electrophysiology of the heart (redrawn from
[28]). The different waveforms for each of the specialized
cells found in the heart are shown. The latency shown ap-
proximates that normally found in the healthy heart.
The accuracy of the R-wave occurrence time estimates is often required to be 1–2 ms and, thus, the
sampling frequency of the ECG should be at least 500–1000 Hz [51]. If the sampling frequency of the
ECG is less than 500 Hz, the errors in R-wave occurrence times can cause critical distortion to HRV
analysis results, especially to spectrum estimates [32]. The distortion of the spectrum is even bigger
if the overall variability in heart rate is small [40]. The estimation accuracy can however be improved
by interpolating the QRS complex e.g. by using a cubic spline interpolation [11] or some model based
approach [6]. Kubios HRV uses interpolation to improve the detection accuracy.
Kubios HRV (ver. 3.0.2)